 Neonatal Diabetes Mellitus (NDM) is a rare disease that may be transient or permanent. KCNJ11 gene mutations represent the most common cause of Permanent NDM but are only rarely implicated in Transient NDM – the motive behind this phenomenon is still unclear. Genetic diagnosis of NDM patients affects management strategy choices, as exemplified by the particularly successful use of exclusive sulfonylurea treatment on KCNJ11-related NDM. We present 2 case reports of patients that, despite having the same presenting condition and being later found to have the same mutated gene, had significantly different outcomes. While one illustrates the importance of genetic testing on therapeutic choices, the other shows the test’s limitation when it comes to predicting the patients’ final outcome – showing that even the most prevalent cause of permanent NDM can cause transient forms of the condition. For more information click here.
Neonatal Diabetes Mellitus (NDM) is a rare disease that may be transient or permanent. KCNJ11 gene mutations represent the most common cause of Permanent NDM but are only rarely implicated in Transient NDM – the motive behind this phenomenon is still unclear. Genetic diagnosis of NDM patients affects management strategy choices, as exemplified by the particularly successful use of exclusive sulfonylurea treatment on KCNJ11-related NDM. We present 2 case reports of patients that, despite having the same presenting condition and being later found to have the same mutated gene, had significantly different outcomes. While one illustrates the importance of genetic testing on therapeutic choices, the other shows the test’s limitation when it comes to predicting the patients’ final outcome – showing that even the most prevalent cause of permanent NDM can cause transient forms of the condition. For more information click here.
Featured posts
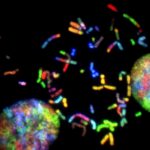 Most patients with rare diseases do not receive a molecular diagnosis and the aetiological variants and causative genes for more than half such disorders remain to be discovered. Here we used whole-genome sequencing (WGS) in a national health system to streamline diagnosis and to discover unknown aetiological variants in the coding and non-coding regions of the genome. We generated WGS data for 13,037 participants, of whom 9,802 had a rare disease, and provided a genetic diagnosis to 1,138 of the 7,065 extensively phenotyped participants. We identified 95 Mendelian associations between genes and rare diseases, of which 11 have been discovered since 2015 and at least 79 are confirmed to be aetiological. By generating WGS data of UK Biobank participants, we found that rare alleles can explain the presence of some individuals in the tails of a quantitative trait for red blood cells. Finally, we identified four novel non-coding variants that cause disease through the disruption of transcription of ARPC1B, GATA1, LRBA and MPL. Our study demonstrates a synergy by using WGS for diagnosis and aetiological discovery in routine healthcare. For more information click here.
Most patients with rare diseases do not receive a molecular diagnosis and the aetiological variants and causative genes for more than half such disorders remain to be discovered. Here we used whole-genome sequencing (WGS) in a national health system to streamline diagnosis and to discover unknown aetiological variants in the coding and non-coding regions of the genome. We generated WGS data for 13,037 participants, of whom 9,802 had a rare disease, and provided a genetic diagnosis to 1,138 of the 7,065 extensively phenotyped participants. We identified 95 Mendelian associations between genes and rare diseases, of which 11 have been discovered since 2015 and at least 79 are confirmed to be aetiological. By generating WGS data of UK Biobank participants, we found that rare alleles can explain the presence of some individuals in the tails of a quantitative trait for red blood cells. Finally, we identified four novel non-coding variants that cause disease through the disruption of transcription of ARPC1B, GATA1, LRBA and MPL. Our study demonstrates a synergy by using WGS for diagnosis and aetiological discovery in routine healthcare. For more information click here.
 For an endocrinologist, nephrogenic diabetes insipidus (NDI) is an end-organ disease, that is the antidiuretic hormone, arginine-vasopressin (AVP) is normally produced but not recognized by the kidney with an inability to concentrate urine despite elevated plasma concentrations of AVP. Polyuria with hyposthenuria and polydipsia are the cardinal clinical manifestations of the disease. For a geneticist, hereditary NDI is a rare disease with a prevalence of five per million males secondary to loss of function of the vasopressin V2 receptor, an X-linked gene, or loss of function of the water channel AQP2. These are small genes, easily sequenced, with a number of both recurrent and private mutations described as disease causing. Other inherited disorders with mild, moderate or severe inability to concentrate urine include Bartter’s syndrome and cystinosis. MAGED2 mutations are responsible for a transient form of Bartter’s syndrome with severe polyhydramnios. The purpose of this review is to describe classical phenotype findings that will help physicians to identify early, before dehydration episodes with hypernatremia, patients with familial NDI. A number of patients are still diagnosed late with repeated dehydration episodes and large dilations of the urinary tract leading to a flow obstructive nephropathy with progressive deterioration of glomerular function. Families with ancestral X-linked AVPR2 mutations could be reconstructed and all female heterozygote patients identified with subsequent perinatal genetic testing to recognize affected males within 2 weeks of birth. Prevention of dehydration episodes is of critical importance in early life and beyond and decreasing solute intake will diminish total urine output. For more information click here.
For an endocrinologist, nephrogenic diabetes insipidus (NDI) is an end-organ disease, that is the antidiuretic hormone, arginine-vasopressin (AVP) is normally produced but not recognized by the kidney with an inability to concentrate urine despite elevated plasma concentrations of AVP. Polyuria with hyposthenuria and polydipsia are the cardinal clinical manifestations of the disease. For a geneticist, hereditary NDI is a rare disease with a prevalence of five per million males secondary to loss of function of the vasopressin V2 receptor, an X-linked gene, or loss of function of the water channel AQP2. These are small genes, easily sequenced, with a number of both recurrent and private mutations described as disease causing. Other inherited disorders with mild, moderate or severe inability to concentrate urine include Bartter’s syndrome and cystinosis. MAGED2 mutations are responsible for a transient form of Bartter’s syndrome with severe polyhydramnios. The purpose of this review is to describe classical phenotype findings that will help physicians to identify early, before dehydration episodes with hypernatremia, patients with familial NDI. A number of patients are still diagnosed late with repeated dehydration episodes and large dilations of the urinary tract leading to a flow obstructive nephropathy with progressive deterioration of glomerular function. Families with ancestral X-linked AVPR2 mutations could be reconstructed and all female heterozygote patients identified with subsequent perinatal genetic testing to recognize affected males within 2 weeks of birth. Prevention of dehydration episodes is of critical importance in early life and beyond and decreasing solute intake will diminish total urine output. For more information click here.
 The term Meniere disease (MD) gathers a set of rare diseases involving the inner ear characterized by episodic vertigo associated with fluctuating auditory symptoms. Five clinical subgroups of patients have been defined, including familial MD, autoimmune MD, and MD with migraine. The diagnosis is based on clinical criteria as no biomarker is available, but genetic factors have a significant contribution in familial and non-familial MD. In this review, the authors summarize the pharmacological treatment for vertigo in MD, providing evidence from preclinical and clinical studies. However, evidence supporting the efficacy for betahistine, diuretics, and intratympanic administration of corticosteroids or gentamicin is limited. For more information click here.
The term Meniere disease (MD) gathers a set of rare diseases involving the inner ear characterized by episodic vertigo associated with fluctuating auditory symptoms. Five clinical subgroups of patients have been defined, including familial MD, autoimmune MD, and MD with migraine. The diagnosis is based on clinical criteria as no biomarker is available, but genetic factors have a significant contribution in familial and non-familial MD. In this review, the authors summarize the pharmacological treatment for vertigo in MD, providing evidence from preclinical and clinical studies. However, evidence supporting the efficacy for betahistine, diuretics, and intratympanic administration of corticosteroids or gentamicin is limited. For more information click here.
 New therapeutic approaches have been established in the field of rare skeletal diseases (e.g., for osteogenesis imperfecta, achondroplasia, hypophosphatemic rickets, hypophosphatasia, and fibrodysplasia ossificans progressiva). After elucidation of the underlying genotypes and pathophysiologic alterations of these diseases, new treatment options have been designed. Most drugs are based on an interaction with the disease-specific cascade of enzymes and proteins involved in the disease. Thereby an approved treatment is available for children with severe forms of hypophosphatasia and hypophosphatemic rickets (asfotase alfa, burosumab). Additionally, there are different phase 3 trials ongoing assessing the efficacy and safety of drugs for osteogenesis imperfecta, achondroplasia, and fibrodysplasia ossificans progressiva (denosumab, vosoritide, palovarotene).Because all these diseases are rare, the number of investigated patients in the trials is small, and the knowledge about rare side effects and long-term outcome is limited. Therefore it is recommended to treat the patients in specialized centers where the effects of the drugs can be evaluated and data about safety, side effects, and efficacy can be collected.Based on the fact that most drugs for rare diseases are highly expensive clear indications for start of a treatment, evaluation of the therapy and recommendations how long a treatment has to be administrated are urgently needed. For more information click here.
New therapeutic approaches have been established in the field of rare skeletal diseases (e.g., for osteogenesis imperfecta, achondroplasia, hypophosphatemic rickets, hypophosphatasia, and fibrodysplasia ossificans progressiva). After elucidation of the underlying genotypes and pathophysiologic alterations of these diseases, new treatment options have been designed. Most drugs are based on an interaction with the disease-specific cascade of enzymes and proteins involved in the disease. Thereby an approved treatment is available for children with severe forms of hypophosphatasia and hypophosphatemic rickets (asfotase alfa, burosumab). Additionally, there are different phase 3 trials ongoing assessing the efficacy and safety of drugs for osteogenesis imperfecta, achondroplasia, and fibrodysplasia ossificans progressiva (denosumab, vosoritide, palovarotene).Because all these diseases are rare, the number of investigated patients in the trials is small, and the knowledge about rare side effects and long-term outcome is limited. Therefore it is recommended to treat the patients in specialized centers where the effects of the drugs can be evaluated and data about safety, side effects, and efficacy can be collected.Based on the fact that most drugs for rare diseases are highly expensive clear indications for start of a treatment, evaluation of the therapy and recommendations how long a treatment has to be administrated are urgently needed. For more information click here.
 Children’s interstitial and diffuse lung diseases are a diverse group of rare lung disorders that present in childhood with diffuse pulmonary infiltrates and respiratory signs and symptoms. Children with these disorders face high morbidity and mortality and their families must cope with overwhelming uncertainty. Physicians caring for these patients are challenged by a paucity of directed therapies, or even understanding of natural history. Through the establishment of the Children’s Interstitial Lung Disease Foundation Research Network and the Children’s Interstitial Lung Disease Foundation significant progress has been made through collaboration and research. This review outlines the past and current successes in the new and rapidly growing field of Children’s Interstitial and Diffuse Lung Disease. For more information click here.
Children’s interstitial and diffuse lung diseases are a diverse group of rare lung disorders that present in childhood with diffuse pulmonary infiltrates and respiratory signs and symptoms. Children with these disorders face high morbidity and mortality and their families must cope with overwhelming uncertainty. Physicians caring for these patients are challenged by a paucity of directed therapies, or even understanding of natural history. Through the establishment of the Children’s Interstitial Lung Disease Foundation Research Network and the Children’s Interstitial Lung Disease Foundation significant progress has been made through collaboration and research. This review outlines the past and current successes in the new and rapidly growing field of Children’s Interstitial and Diffuse Lung Disease. For more information click here.
 Neurofibromatosis type 1 (NF1) is an inherited disease characterized by skin hyperpigmentation (most commonly café au lait), multiple tumors in the central and peripheral nervous system, vascular changes, and cognitive impairments. NF1 is predominantly inherited disease, affecting both genders, and in half of the cases it is a de novo mutation. There is a great variability of the disease manifestations even among members of the same family. Life expectancy in patients with NF1 is reduced by 10-15 years on average, with malignancies being the most common cause of death. Even though there are established clinical diagnostic criteria, more than a half of sporadic cases may remain unrecognized in early childhood. Recently, an improvement of the NF1 diagnosis has been observed due to increased awareness and implementation of advanced molecular – genetic and imaging technologies. Patients with NF1 need adequate care and must be monitored closely by competent healthcare professionals utilising a multidisciplinary approach. This publication aims to analyze the available epidemiological data on NF1, as well as to provide an insight into NF1 prevalence in Bulgaria. For more information click here.
Neurofibromatosis type 1 (NF1) is an inherited disease characterized by skin hyperpigmentation (most commonly café au lait), multiple tumors in the central and peripheral nervous system, vascular changes, and cognitive impairments. NF1 is predominantly inherited disease, affecting both genders, and in half of the cases it is a de novo mutation. There is a great variability of the disease manifestations even among members of the same family. Life expectancy in patients with NF1 is reduced by 10-15 years on average, with malignancies being the most common cause of death. Even though there are established clinical diagnostic criteria, more than a half of sporadic cases may remain unrecognized in early childhood. Recently, an improvement of the NF1 diagnosis has been observed due to increased awareness and implementation of advanced molecular – genetic and imaging technologies. Patients with NF1 need adequate care and must be monitored closely by competent healthcare professionals utilising a multidisciplinary approach. This publication aims to analyze the available epidemiological data on NF1, as well as to provide an insight into NF1 prevalence in Bulgaria. For more information click here.
 Angiolipomas are rare benign lipomatous lesions that differ from lipoma in their characteristic histology, consisting of mature adipocytes and prominent, proliferated, thin-walled blood vessels. They occur before puberty or in young adults and are usually presented as multiple, painful, slow-growing, small nodules located in the subcutaneous tissue of the forearm or elbows. Although they can be seen anywhere on the body, they are rare in the head and neck area. Treatment of angiolipomas requires a complete surgical excision. In the present report, we describe a rare case of angiolipoma of the back of the head in a 65-year-old woman. For more information click here.
Angiolipomas are rare benign lipomatous lesions that differ from lipoma in their characteristic histology, consisting of mature adipocytes and prominent, proliferated, thin-walled blood vessels. They occur before puberty or in young adults and are usually presented as multiple, painful, slow-growing, small nodules located in the subcutaneous tissue of the forearm or elbows. Although they can be seen anywhere on the body, they are rare in the head and neck area. Treatment of angiolipomas requires a complete surgical excision. In the present report, we describe a rare case of angiolipoma of the back of the head in a 65-year-old woman. For more information click here.
 Impacted tooth is one that has not fully or partially erupted and is “retained” in its eruption, remaining in the bone in the wrong position against another tooth, bone, or soft tissue, so that further eruption is unlikely. This condition is most common in third molars and is thought to be found in about 73% of young adults in Europe. Dentigerous cyst is the second most common odontogenic cyst and represents about 20-24% of all odontogenic cysts of the jaws. These cysts usually remain asymptomatic and rarely reach large sizes and displace the associated tooth. In our article we present four cases of impacted third molars with atypical localization and concomitant large dentigerous cysts. A brief review of the literature with similar findings is presented, as well as the different approaches to the treatment of these cases. For more information click here.
Impacted tooth is one that has not fully or partially erupted and is “retained” in its eruption, remaining in the bone in the wrong position against another tooth, bone, or soft tissue, so that further eruption is unlikely. This condition is most common in third molars and is thought to be found in about 73% of young adults in Europe. Dentigerous cyst is the second most common odontogenic cyst and represents about 20-24% of all odontogenic cysts of the jaws. These cysts usually remain asymptomatic and rarely reach large sizes and displace the associated tooth. In our article we present four cases of impacted third molars with atypical localization and concomitant large dentigerous cysts. A brief review of the literature with similar findings is presented, as well as the different approaches to the treatment of these cases. For more information click here.
Pathological mandibular fracture as a complication after lower third molar extraction in a patient with osteonecrosis
 We present a case of a male patient admitted for emergency treatment at the Clinic for Maxillofacial Surgery of the University Hospital “St. George” in Plovdiv with suspected lower jaw fracture. The patient had previous nephrectomy for renal cancer in 2016. Bone metastases were detected in 2017 and therapy with Zometa was undertaken. In 2018 the patient was diagnosed with osteonecrosis of the mandible. The patient reports that he has been treated at another Clinic for Maxillofacial Surgery for extraction of impacted wisdom tooth. A few days after the removal of the threads during feeding, a strong cracking noise was heard in the region of the jaw angle at the side of the extraction. An orthopantomogram and computed tomography were performed, which revealed a pathological fracture. For more information click here.
We present a case of a male patient admitted for emergency treatment at the Clinic for Maxillofacial Surgery of the University Hospital “St. George” in Plovdiv with suspected lower jaw fracture. The patient had previous nephrectomy for renal cancer in 2016. Bone metastases were detected in 2017 and therapy with Zometa was undertaken. In 2018 the patient was diagnosed with osteonecrosis of the mandible. The patient reports that he has been treated at another Clinic for Maxillofacial Surgery for extraction of impacted wisdom tooth. A few days after the removal of the threads during feeding, a strong cracking noise was heard in the region of the jaw angle at the side of the extraction. An orthopantomogram and computed tomography were performed, which revealed a pathological fracture. For more information click here.
